Endometriosis Diagnosis
How is Endometriosis Diagnosed?
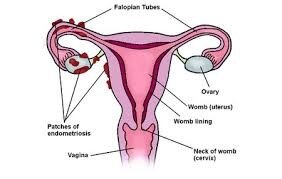
It is estimated that 170-200 million women are affected by endometriosis worldwide. That’s around 1 in 10 women. It typically affects women during their reproductive years between the ages of 15 to 49, with the risk of developing the disease increasing with age. Although very rare presentations, endometriosis has been described in young girls, in women who have already reached menopause and even in some men who take large doses of oestrogen.
While many women experience the common symptoms of endometriosis, a large proportion of women with the disease either have no symptoms or experience atypical symptoms, making it difficult for doctors to suspect the disease and delaying the diagnosis.
Diagnosis of endometriosis often takes up to 7 – 10 years from the onset of symptoms. This is because of a combination of factors which include lack of awareness about the disease or inexperience of doctors in primary care, normalisation of endometriosis pain as “part of being a woman” and lack of an easy and precise method of diagnosis.
Early detection of the condition is important as it has the potential to reduce long-term impact and improve quality of life, as well as better management and prevention of infertility.
History and physical examination
A careful history and examination by a trained physician can suggest the presence of the disease. Stage 1 or mild endometriosis usually cannot be felt on examination, however in more advanced stages, when there are nodules or cysts, can be detected during a gynaecological assessment.
Ultrasound
Ultrasound is the principal mode of imaging used for the pelvis as it is very effective and sensitive to assess the uterus and ovaries. It also has the advantage of being non-invasive and available in most places.
To assess endometriosis however, it requires specific and advanced training. Not all ultrasonographists have the training required to be able to detect endometriosis. Also, most superficial endometriotic lesions are not visible on ultrasound. The ultrasound can show endometriosis in cases where there are endometriotic cysts on one or both ovaries (endometrioma), when there are nodules of deep infiltrating disease or when the endometriosis has caused adhesions or scarring.
Magnetic Resonance Imaging
MRI is another useful resource to assess endometriosis. Similar to the ultrasound, it does not show superficial endometriotic lesions, but can be very useful to assess more severe forms of the disease when there are ovarian cysts or nodules affecting the vagina, the rectum or the bladder. It is also useful to diagnose extra pelvic endometriosis such as in the lungs or diaphragm.
It also relies on the training and experience of the radiologist. MRI is currently more expensive and not as available as ultrasound.
Blood tests
A simple, non-invasive test would be most welcomed by patients and health professionals alike, hence why there has been a lot of research trying to find a blood test that can diagnose endometriosis. Unfortunately, to date, there is no reliable blood test to diagnose the disease.
CA 125 is a protein that is found in greater concentration in tumour cells than in other cells of the body. Women with ovarian cancer can have high levels of CA 125 in the blood.
Although some women with endometriosis also show high levels of CA 125, the test is not specific and not reliable to diagnose endometriosis. At present, it is not routinely used to diagnose the disease.
In 2019, a British company, MDNA Life Sciences, published early reports of what was going to be a promising blood test, able to diagnose endometriosis in 90% of women with the condition. Unfortunately, the Mitotic Endometriosis Test has not lived up to the hype and it is still not available.
Laparoscopy
The gold standard for definitive diagnosis of endometriosis is still a laparoscopy, also known as keyhole surgery, where a camera is inserted into the abdomen through a small incision in the umbilicus.
Endometriotic lesions can then be seen by the surgeon, samples can be taken and sent through to pathology. Histopathologic (biopsy) evidence is the definitive confirmation of the disease.
The main advantage of the laparoscopy is that it is not only diagnostic, but also the treatment for endometriosis. All lesions seen during the procedure can be excised. Please see the laparoscopy and endometriosis treatment pages for more detail.
A laparoscopy is not always mandatory as sometimes it is OK not to have a definitive diagnosis of endometriosis. This is true when:
The symptoms are not very severe and do not have a significant impact in the woman’s quality of life.
The symptoms respond well to medical treatment.
The woman is able to fall pregnant without treatment or is not trying to conceive.
A good quality ultrasound does not show ovarian cysts or deep infiltrating endometriotic nodules.